Understanding Irritable Bowel Syndrome (IBS) and Its Influence on Endurance Athletes
As an endurance athlete, consistency with training allows you time to nail down key strategies for obtaining optimal performance at your goal event. A few things to focus on are building endurance, mental toughness, and adequate fueling through nutrition and hydration. If you have Irritable Bowel Syndrome (IBS), then nutrition and hydration are even more crucial to prevent flare-ups and setbacks in training.
Understanding Irritable Bowel Syndrome (IBS) and the Impact on Endurance Athletes
What is Irritable Bowel Syndrome? Well, to make it simple, it is when the stomach and intestines get irritated due to food moving too quickly or too slowly through the gastrointestinal tract. Stress can also irritate the nerves that line the wall of your gut and become over-sensitized. This is important for endurance athletes to know and understand. The endurance activity in itself can cause food to move too quickly or too slowly through the GI tract based on what you eat and when you eat it in relation to your activity. When this happens, you can have bloating, gas, cramping, abdominal pain, diarrhea, or constipation. This can cause a pause in your training plan for one day or up to a whole week, depending on the severity of your symptoms.
There are ways you can prevent this from happening or at least have some control over the severity of your symptoms. A great first step is tracking trigger foods- identifying and removing them from your diet.
After this step, if you still have issues, I suggest trying an elimination diet, such as Low FODMAP, to rule out food families or known GI irritants.
Embracing a Low-FODMAP Diet: A Personalized Approach to IBS Management
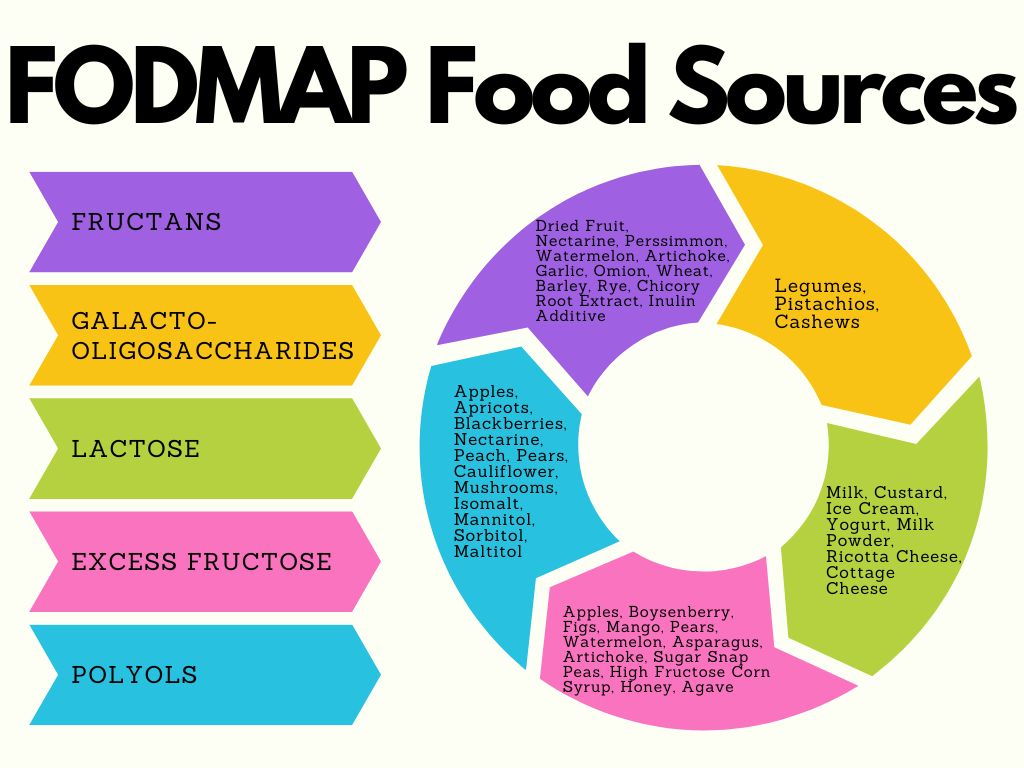
FODMAPs are sugars found in foods, specifically fermentable oligosaccharides (fructans and galacto-oligosaccharides – GOS), disaccharides (lactose and milk sugar), monosaccharides (excess fructose), and polyols (sugar alcohols).
FODMAPS can produce symptoms in individuals with IBS because they pull water into the GI tract, which can lead to diarrhea. When eaten in excess, they also ferment by your naturally occurring gut bacteria, creating gas, bloating, cramping, and abdominal pain.
Following a Low FODMAP diet can allow you to determine foods and food families that may be a trigger for digestive assault. I suggest following the elimination phase between training cycles, but if that is not in the foreseeable future, aim for the first few weeks of your training cycle. That way, you are still in lower mileage with less caloric demand than when you are further along, and your body needs all the food for refueling. The elimination phase generally lasts between 2-4 weeks and then you start reintroducing foods back into your diet. Trying to do an elimination diet when you are close to your goal race will inevitably add extra stress, let alone limit the food sources you can otherwise use for fuel.
Balancing Nutrition for Endurance Performance: Meeting Energy Demands and Digestive Needs
Once you have determined what foods to limit or eliminate from your diet, then you can begin adequately fueling your body for training. One of the most important macronutrients to consume for endurance activities are carbohydrates. With FODMAPs coming mostly from carbohydrate sources, the last thing you want to do is consume a food that will continuously trigger your IBS symptoms.
Meal timing around training is key. Pre-, during, and post-workout fueling optimizes your outcomes. Using your training cycle to try new things is ideal, as you never want to change up the plan on race day. For pre-workout fueling, you want to aim for good timing and appropriate balance. Having something 1-2 hours prior to activities allows your body time to digest and the ability to convert food into glycogen for energy in your muscles. This is assuming your workout is in the morning. If you work out in the afternoon, then eating regularly throughout the day will be enough to replenish your glycogen stores.
Personally, I have had to recognize foods that trigger my IBS for my afternoon workouts. On the days I have a key workout, I am careful to avoid any trigger foods prior to my run to prevent a “gut bomb” while out on the trail. On long run days I have trialed a few different nutrition sources to consume while I am running. Through trial and error, I have been able to nail down what works best for me. This is a common practice among endurance athletes; part of training is testing out nutrition as well. It is better to find what does and does not work while training instead of at the goal event.
Post-workout or post-race recovery is also important. Continuing to focus on carbohydrates immediately is key to replenishing your muscle glycogen stores. What does this mean? Glycogen is the stored form of glucose and one of the main fuel sources for muscles. Adding protein is helpful for cell structure and rebuilding/repairing fatigued muscles. Make sure you are checking the food or supplement labels on the products you are using to ensure they do not contain ingredients that may be a trigger for an IBS flare.
Seeking Professional Guidance: A Personalized Approach to Nutrition and IBS
Taking on the task of managing your nutrition and understanding your symptoms can be daunting. If you have tried a few things and feel like you are still spinning your wheels without much progress then maybe it is time to look to a professional. Find an outpatient dietitian in your area, or if you are tech-savvy, many dietitians can offer virtual/telehealth appointments. Dietitians are nutrition professionals who can help you with navigating the Low FODMAP diet, fueling your endurance training, and assisting in managing your IBS symptoms and flare-ups, among other nutrition areas. You do not have to try to figure this out on your own.
- Low Fodmap Diet. Stanford Health Care. (2017, September 12).
- Mayo Foundation for Medical Education and Research. (2023, May 12). Irritable bowel syndrome. Mayo Clinic.


















Comments
Join The Conversation...